I recorded audio of the following presentation by my father at Beth Israel Deaconess Medical Center in Boston in January 2020 and later worked with him to incorporate the slides and post it as a video. The video not only gives a history of major developments in gastroenterology from 1965-2020, but also gives insights into how crucial discoveries and paradigm shifts (including those in other fields) can upend the established order. A transcript is included below.
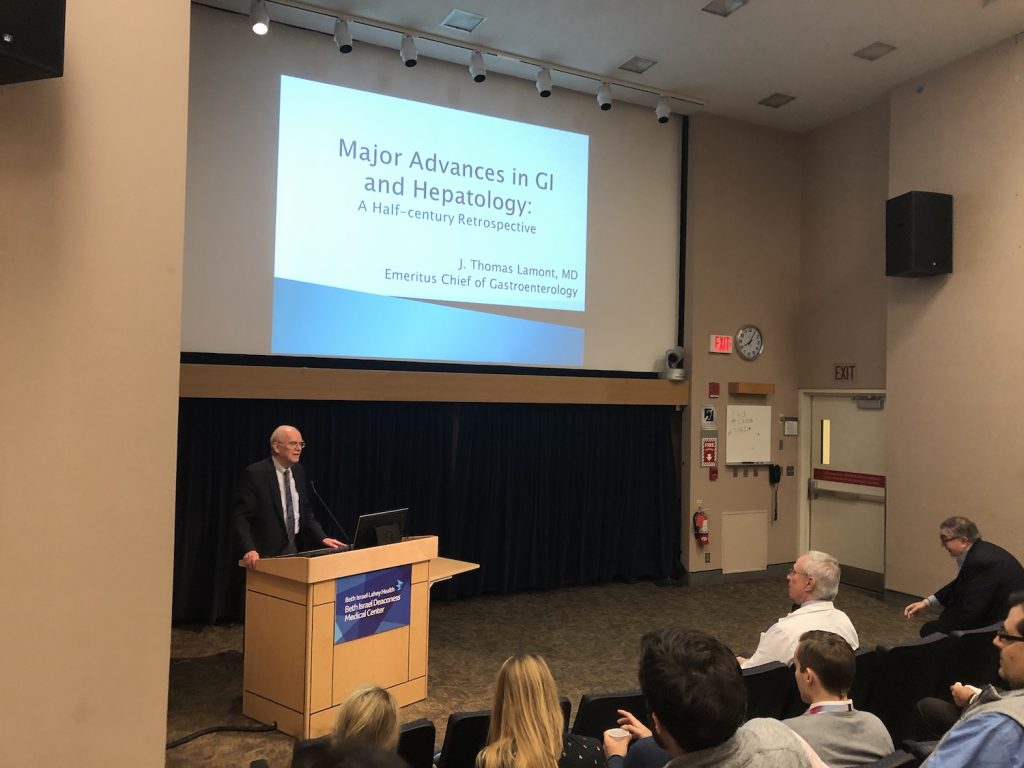
Medical Grand Rounds: Major Advances in GI & Hepatology: A Half-Century Retrospective.
Presented by J. Thomas Lamont, MD (Rabb Professor of Medicine at Harvard Medical School). Sherman Auditorium, Beth Israel Deaconess Medical Center, Boston, January 9, 2020.
Introduction by Nezam H. Afdhal, MD:
The Zetzel Visiting professor lecturer this year is Professor Thomas Lamont, who is, as you all know, the Emeritus Chief of Gastroenterology at BIDMC. Tom started his career at UCLA, where he did his residency, and then has the dubious distinction of having worked at every teaching hospital in the Boston area, except Tufts.
After his fellowship at MGH was on the Faculty at Harvard Medical School until 1980, when he became the chief of GI at Boston Medical Center. He then came to BIDMC to be the Chief of Gastroenterology in 1996. His career has spanned major achievements in all areas of gastroenterology. Many of you don’t know this, but he was one of the first people who worked out how gall stones developed in the gallbladder.
He published a paper that was the cover of Nature that illustrated why the stomach does not digest itself due to the interactions of mucins and the effect of acid on the mucin structure within the stomach. At BIDMC he and his research team worked on the mechanism of action of the toxins for C. difficile. These are just some of his scientific advances. He is a clinician, still sees patients today, and is a well sought after teacher, and has educated innumerable fellows and faculty. He’s been a mentor to many. He’s been a great friend to the GI division here at BIDMC. His lecture this morning is going to be a look back at what has happened in the 50 years of Tom’s career in gastroenterology. ,
Dr J. Thomas Lamont, MD:
This is the UCLA Medical Center where I was an intern in 1965. During my training there I thought that the wisdom and knowledge that I was taught was really top level. Looking back now, I realize that all of it has been wiped away, or superseded by new knowledge .What I was taught then was thought to be state of art, but eventually the bulk of it was discarded and replaced by more accurate and improved medical science
I used to think, and a lot of people believe that discoveries are incremental, that knowledge is added like bricks to a wall which you gradually build. But in fact scientific discoveries are primarily revolutionary not incremental. There’s a paradigm shift which is a radical change in the way we do things. It’s often disruptive, a word borrowed from technology, where the new discovery or invention blows up whatever was there before. Later in the talk I’ll show you some examples of disruptive discoveries and inventions in the field of Gastroenterology.
A major feature in the field of scientific discovery is resistance from the establishment. I can tell you that Boston has a very powerful medical establishment, and the resistance to some of what I’m going to show you was quite robust. So, if you’re interested in this topic, there’s a very important small book, about 100 pages long, by Thomas Kuhn called “The Structure of Scientific Revolutions”. Kuhn championed the concept of paradigm shift, in which scientists have to move away from something that has been accepted for a long, long time. And the new paradigm replaces the original paradigm, which eventually fades away.
For example, an original paradigm in GI was, “excessive gastric acid secretion causes duodenal ulcers”. This paradigm is what we thought up until about the late ’80s. But then we gradually learned that in fact Helicobacter pylori infection is the cause of the majority of duodenal ulcers.
Here is an overview about some of the major discoveries I’m going to talk about. There’s dozens of things that could be discussed at a talk like this, and I’m not even sure I’ll be able to get through the ones I put in the timeline here. I’m going to start with fiberoptic endoscopy, because I think that had the biggest influence on our specialty, and defined what it is today. The discovery of H2 acid blockers was a major advance, followed around the same time by the discovery of the role of Helicobacter, and the invention of proton pump inhibitors. The major discoveries in Hepatitis C virus infection have taken us to the point where this disease is now curable .
If you were a patient in 1820 in Italy, your doctor might approach you with one of these instruments, and it would certainly put the fear of God in you. You can imagine that this urethroscope might be quite uncomfortable. especially as the procedure was performed without pre-medication or sterility.
The GI tract is curvy. That’s the problem with these early endoscopes: they’re not flexible but rigid. Illustrated hers is the type of gastroscope that was still in use in Los Angeles when I was an intern. You can see the gastroscope there over Dr Schindler’s right arm. On his right is Mrs. Schindler who attended every endoscopy and who assisted in moving the patient’s head. During the procedure the patient’s neck would be hyper-extended to allow introduction of the metal endoscope. As you know the esophagus is straight; that’s the only reason why this technique worked at all. The scope couldn’t go around any curves and it was really quite a difficult and even brutal test.
These metal sigmoidoscopes were in daily use up until about 1985 or even 1990 at Boston teaching hospitals. We used plastic scoped that were disposable and every GI fellow and internal medicine residents learned how to do proctoscopy for colon cancer screening.
In 1842 a critical experiment establishes that light could be bent. As shown here a bead of light is transmitted through a tank of water, and you can see that the light follows the curvature of the water as it exits the container. The light actually bounces or is refracted off the side of the column of water. The next big discovery was the development by Narinder Singh Kapany of fiber optic cable, which eventually replaced metal cables and had a huge impact on the field of telecommunications.
Kapany and colleagues then had the idea that extremely thin flexible glass fibers could transmit endoscopic images. This was picked up by Basil Hirschowitz, a native of south Africa, who in 1953 was a GI fellow at the University of Michigan. He was already trained in endoscopy in England before he went to Michigan. Hirschowitz was trained in the Schindler type of endoscopy that I showed you earlier, but he realized that this older technology was difficult and dangerous because of the rigidity of the Schindler scope.
Hopkins and Kapany published a paper in Nature entitled “A Flexible Fiberscope Using Static Scanning.” What they reported was a flexible endoscope that transmitted light through 10,000fiberglass rods that were slightly bigger than a hair. The exciting new and innovative aspect of this paper was the fact that the endoscope was flexible, and that when the scope was bent the image was not distorted.
Hirschowitz heard about this paper from a cardiology resident who had heard about it at journal club in London. Hirschowitz flew to London, met Kapany and Hopkins in a pub, and discussed their invention. They were very encouraging to Hirschowitz and gave him a few glass fibers to take back to Ann Arbor. Hirschowitz returned to his fellowship at Michigan and built the first fiberoptic gastroscope with help from Larry Curtis and Wilbur Peters who were physicists. After a few years of trial and error, they produced the first gastroscope
GI doctors in the audience will notice there’s no wheels on this first scope, so it’s not steerable. It’s a side-viewing scope which makes it really difficult to insert. compared to what we have today, it is not very practical or useful. But this invention marked the beginning of fiberoptic endoscopy.
Hirschowitz, like a lot of fellows and young researchers in science, first tested the device on himself in February 1957. He managed to control his own gag reflex, passed through his esophagus and looked around in his own stomach. He then scoped a patient indicated on the slide as patient #2. A most remarkable aspect of this discovery was that it was not supported by grants and was carried out by a GI fellow, and two physicists who worked very hard to create this incredible advance.
Dr Hirschowitz then linked up with American Cystoscope Manufacturing Inc. an American device company that made rigid Urologic scopes who produced this first commercial fiberoptic gastroscope. Again, it had no wheels to allow steering, but it had an air channel and the optics were good enough to allow examination of most of the stomach. Hirschowitz himself published this seminal paper in Lancet in May of ’61 that described his experiences in a series of patients he examined with the new scope. In the next to last sentence he challenged the existing paradigm. “The conventional gastroscope ( Schindler gastroscope) has become obsolete on all counts.”
The invention of endoscopy was not a hard sell. Some of the other things I’m going to talk about later were met with strong opposition, but fiberoptic flexible endoscopy was widely and quickly accepted. By the time I was a GI fellow in 1971 and into the early ‘1980s gastroscopes had was being taught at all the Boston teaching hospitals. The opposition was not to the scope itself, but rather to the idea of fellows leaving the laboratory and learning what sounded like a surgical technique.
Certain research-oriented professors at Harvard were somewhat opposed to this. One of my mentors said to me,, “Once they taste blood, they’re gone forever.” He meant that once GI fellows had used the scope to diagnose a GI bleeder they would lose their interest in basic research.”
The impact of fiberoptic endoscopy on practice was massive. Currently about 100-million endoscopies performed a year in the United States, about two thirds of them by GI doctors. Flexible fiberoptic endoscopy has had important impact worldwide in many medical and surgical fields.
This slide compares how we treated common GI diseases at UCLA in 1965, and how we handles these conditions currently. For example patients with GI bleeding that did not respond to antacid therapy typically went to surgery. Nowadays we manage this situation with proton pump inhibitors, and if bleeding continues or is torrential then we manage the situation endoscopically. Variceal hemorrhage was a fearsome occurrence in the mid 1960s and if persistent life-threatening was referred for a portocaval shunt. Currently this operation is seldom performed here, and we rely almost entirely on endoscopic control of variceal bleeding and radiologic placement of portocaval shunts or TIPS.
Management of obstructive jaundice was very difficult because we did not have any imaging studies to examine the bile ducts. Sometimes we resorted to so- called steroid whitewash especially if you were afraid of doing an laparotomy. This involved administration of corticosteroids for a week. If the jaundice improved then it was likely not mechanical obstruction but hepatitis or some other form of cholestatic jaundice for which surgical exploration was not required. Treatment of achalasia typically required either a forceful dilatation of the lower esophagus which was quite dangerous or a surgical myotomy. Currently we can perform a myotomy through the endoscope to treat achalasia at our hospital .
Now I’d like to tell you about a few advances in endoscopy that have been made here in our division. new approach is called molecular endoscopy where the scope can analyze tissue from tumors using laser light scattering.
This approach was developed here by clinical investigators in our GI unit working with Professor Lev Perelman a physicist in the GI division who specializes in photonics. Dr Perlman and colleagues hand-built this equipment which includes a scanner that goes through the biopsy channel of the endoscope. This allows a laser beam to be aimed at the epithelial lining of the esophagus and then measures reflected light from the wall of the esophagus. As the scope is withdrawn the instrument turns so it’s like an internal CT scan of the esophagus, except it’s spectroscopy. The reflected light ia analyzed to detect dysplasia more accurately than the optical techniques and biopsy.
Here is some information on the first prospective randomized clinical study on artificial intelligence to improve colon screening for cancer. This work is being carried out here by Tyler Berzin and Jeremy Glissen-Brown, one of our fellows, and was just published in Gut. They report the ability of artificial intelligence developed through game technology, to assist a physician doing a screening colonoscopy. The main quality outcome of a screening colonoscopy is adenoma detection rate or ADR.The goal is o find all the adenomas and take them out and prevent future development of colon cancer. The arrows indicate the polyp detection rate, or PDR, using routine optical colonoscopy at 29% vs 45 %with the assistance of artificial intelligence. This innovative technology will have huge impact on the ability of endoscopy to find and remove colonic polyps, and will improve our ability to prevent colon cancer.
S Mel Wilcox, the division director at the University of Alabama, where Dr. Hirschowitz spent his career, stated that it Basil Hirschowitz created the field of modern gastroenterology. When I started my training, GI was a reflective, diagnostic, minimally invasive specialty similar to endocrinology. Now the field is closer to urology or ENT than it is to some medical specialties.
I’d like to turn now to story of discovery that started in Australia. Pictured here: a medical resident, the tired-looking fellow on the left. He was working in the Royal Perth Hospital and asked his boss, the head of the GI unit, if he could help him find a suitable research project. — He was becoming interested in gastroenterology, had a curious mind, and was keen to explore although up to then he had never done any research. His boss referred him to Robin Warren, shown here on the right, an assistant professor of pathology at the hospital.
Barry went over one afternoon and sat down with Dr Warren to examine pathology slides that Warren had been collecting from GI patients with gastritis and ulcers. Warren was especially interested in this silver stain of a spiral bacteria that was present in the stomach. Warren recognized that this organism had been described for at least 100 years. But so far it had not been identified or named, and its role in diseases like gastritis and ulcers was unknown to medical science.
Barry Marshall realized that some of the patients that Robin Warren was telling him about were his own patients. He had learned fiberoptic endoscopy, and he was performing biopsies on these same patients and knew their medical histories. So this clinical connection lit a spark, and the two of them teamed up and made a remarkable discovery. What they did was to simply correlate this finding with the presence of active chronic gastritis. They published their first paper, a brief letter to the editor in Lancet in 1983t, which described a series of their patients with active gastritis and the present of this curved bacillus in their stomachs.
They went on then to make further correlations between the curved bacilli and peptic ulcers and eventually gastric cancer. This discovery was innovative and totally new. and was met with huge resistance by the medical establishment. The notion that peptic ulcer was an infectious disease met with near universal rejection. I actually remember the journal club in a Boston teaching hospital near here where this was first presented. The discovery was universally rejected by most of us in attendance. The problem was that in certain parts of the world, 80% of the population were infected. How could something that common be a cause of a disease like peptic ulcer that only occurs in, say, 1% of the population?
Barry Marshall wrote in his note cards and some of his later publication “Everyone was against me, but I knew I was right.” So who was against him? The acid mafia, a powerful group of senior investigators who championed the idea that hydrochloric acid was the key to formation of stomach ulcers. When we were residents and fellows we had to know a lot about gastric hydrochloric acid secretion. So those who believed in the primacy of stomach acid were definitely strongly opposed to these Australian upstarts, Marshall and Warren.
Listed here are Koch’s postulates; the last two are particularly important in establishing the infectious etiology of a given disease. The pure culture, when inoculated into the experimental animals, must reproduce the disease.” “Microorganisms must be recovered from the diseased animal.”
In this instance the experimental subject was Barry Marshal himself He swallowed a pure culture of Helicobacter pylori that he had isolated from one of his patients that he had previously biopsied and cured. So he knew that the strain was treatable and curable. He drank the culture of H pylori and over the next several weeks developed severe acute Helicobacter infection with nausea, vomiting, and severe dyspepsia. He stated that his halitosis was so bad, that his wife told him that he had to sleep on the couch. After the infection was established he treated himself with the anti-Helicobacter therapy and completely recovered. His experiment was soon published in the Medical Journal of Australia in 1985.
Eventually the etiologic role of H pylori in stomach diseases was established without a shadow of doubt. That doesn’t mean that acid doesn’t play an important role in ulcer formation, An old dictum was, “No acid, no ulcer.” That’s pretty much true.
You can easily cure ulcers with proton pump inhibitors. But if you want to cure an ulcer permanently then you have to eradicate Helicobacter. In this study in the New England Journal patients with active duodenal ulcers and Helicobacter infection were first “cured” with, in this case with Tagamet for two weeks, and then they were randomized after the Tagamet was finished to either antibiotics for two weeks to get rid of the Helicobacter or placebo.
You can see here a huge separation of these curves. Without eradication of the H Pylori infection by antibiotics, most patients had recurrence of their ulcers by the end of the study. Many other studies like this finally established the important causative role of this pathogen.
Helicobacter pylori is probably one of the most common infections world wide; in some countries the prevalence overall is about 60- 80%. For example, in Bangladesh about 80% of children are infected by age 5, particularly in areas with poor access to clean food and water. The peptic ulcer rate is about 10% and it turns out to be the cause of a number of important diseases of the stomach and duodenum that are shown on this graphic.
About 100% of patients with Helicobacter get some form of gastritis. It’s not the only cause of gastritis but it’s a major one. Eventually, with chronic, lifelong infection, gastric atrophy may occur. This leads to achlorhydria and in some patients to pernicious anemia with vitamin B-12 deficiency. It’s thought that the majority of stomach cancers result from chronic infection with H pylori. This states that about 1% of infected patients will get gastric cancer. That’s an over-estimate; it’s more like 1 in 1,000, or perhaps even less than that. Infection is also the cause of MALT lymphoma which can be cured by treatment of Helicobacter without chemotherapy, and without removal of the stomach. As already discussedH pylori accounts for the majority of gastric and duodenal ulcers.
Marshall and Warren were finally justified in 2005 when they won the Nobel Prize for Medicine. A couple of blokes from Australia who had not done a lot of research at all, with very little support. they used equipment and tools that were right at hand. This seems to be a study that could have been performed by almost anyone. But they were the first, and their persistence in the face of heavy opposition payed off.
The medical treatments we had for peptic ulcer in the mid 1960s and right up to about mid-’70s was actually very limited and not very effective. The mainstay of medical therapy was antacids. House officers and trainees were expected to know the properties of antacids very well, including doses, and their side effects. We sometimes used a special treatment called the Sippy diet” which consisted of two ounces of cream every half hour alternating with an 30 to 60 ml of an antacid. But a large number of the patients developed severe and semi-acute atherosclerosis from the fat so it was finally abandoned.
At this hospital William Silen and colleagues developed a very unique approach to acute stress ulcers of the stomach with GI hemorrhage in patients in intensive care units. He and his colleagues published a report in a major medical journal that described a technique to reduce the acidity of the stomach. An NG tube was placed in the stomach and the pH was measured. Antacids were instilled through the NG tube to bring the pH above four. This technique was a common treatment for bleeding stress ulcers in that era just prior to the development of effective drugs to block gastric acid secretion.
When antacid therapy failed to heal ulcers and stop bleeding we then turned to surgery. The first thing was to cut the vagus nerve, a vagotamy, and then remove the distal half of the stomach to remove the ulcer and reduce some of the acid-producing cells in the antrum, and then hook up the small intestine. As you can see it’s not very physiologic. There were many side effects. And every GI fellow and house officer had to know the side effects of ulcer operations that were so frequent after these types of operations.
The introduction of acid-blocking drugs truly changed everything. Again there was some push-back from the establishment. Editorials appeared in the New England Journal from internists and surgeons decrying the overuse of acid blocking drugs across America. A quick survey of the in-patient service at Yale New Haven Hospital revealed that 56% of the patients were on an acid blocker. Some of us commented, “Why so low?” Perhaps these meds were over-used but their effectiveness and clinical impact justified widespread use.
Show here is a simplified diagram pf receptor-mediated control of hydrochloric acid secretion. It was known for many years that histamine could strongly stimulate gastric acid secretion. But it was thought that there must be a special receptor for histamine which eventually was called the “histamine 2 receptor.” The gastrin receptor was thought to be a major regulator, and then finally the vagus nerve through acetylcholine, all of them having separate receptors with somewhat different transduction mechanisms. The ultimate step in the acid secretion pathway was the proton pump which secretes a hydrogen ion into the lumen of the gastric gland in exchange for a potassium ion.
Smith, Kline & French started an acid blocker discovery program in 1964 under the leadership of James Black who had already invented and developed propranolol. He was a lead investigator in receptor-mediated physiology and was also an experiences medicinal chemist.
His research team at Smith, Kline & French in the UK finally developed cimetidine, the first billion dollar drug, which hit the market in ’76. It was a blockbuster drug. I was just starting my career as a faculty member and I remember the AGA Digestive Disease Week at that time was all about Tagamet. They were everywhere with it. People were just a-buzz about this new drug. So it was a pretty easy sell except for the over-use that I mentioned.
James Black and colleagues at Smith, Kline & French studied the histamine molecule and then made critical modifications. Substitution of the methyl group on the imidazole ring created an agonist. So that was actually the first discovery. Once you have an agonist — and it did not stimulate H1 receptors — so they knew that they were onto something. It took them about six years to develop this molecule, an H2 blocker which is Tagamet. They had a couple of earlier ones which were very effective but when they tested on patients caused agranulocytosis and pancytopenia. So there were a few missteps but in general it was a very successful campaign.
James Black was awarded the Nobel Prize in 1988 for his discovery of two major drugs: propranolol and H2 acid blockers. He shared the prize with Gertrude Elion and George Hitchings. for their drug development of purine analogs that were used successfully to treat a number of important diseases including autoimmunity, transplant rejection ,infections and gout.,
I would like to say a few more words about Dr. Gertrude Elion. She was born in Brooklyn, went to Hunter College where she started at age 15 and graduated summa cum laude. She then decided to go to graduate school for a PhD. but could not get into a chemistry doctoral program. She was told at one interview by the head of the laboratory, “You might be qualified but you would be a distraction in a lab full of men.”
She then worked for the A&P supermarket company testing the acidity of pickles. Dr Elion finally joined Burroughs Wellcome in 1944 at age 26 as an assistant to George Hitchings with whom she shared the Nobel Prize. She never received a Ph.D, but was awarded many honorary Ph.D.s including one from Harvard
Elion and Hitching developed these drugs two of which, mercaptopurine and azathioprine were used in gastroenterology. They developed the antibiotic trimethoprim, acyclovir, and the others listed there. These are all actually still in use in some form or another. All of these novel drugs were based on modifications of the purine molecule.
When I read about Gertrude Elion I became curious about how many women won the Nobel Prize. Of the 943 Nobel laureates awarded since 1901, only 53 were women. And the graphic shows by 20-year segments that the number of women awardees is slowly rising. In the last 20 years from 2001 to o 2018, the number has increased from previous 20 year segments. The trend is in the right direction and I suspect it will improve over the next 50 years.
Hepatology in the mid 1960s was not very well developed. I can basically summarize what we had then as nothing. We could measure AST and ALT, bilrubin, and Alkaline Phosphatase, and prothrombin time and albumin. We had no imaging, of any kind. As I mentioned before we frequently resorted to exploratory laparotomy as a major diagnostic test.
There were few effective treatments for cirrhosis. I remember one of my teachers I think in residency or perhaps for the fellowship saying that the prognosis of a patient with cirrhosis when you have a complication such as bleeding, ascites or infection was about the same as a person with stage 4 metastatic lung cancer which at that time was not very treatable. Our knowledge of viral hepatitis was quite limited. We used descriptive terms for such as infectious hepatitis, short incubation hepatitis, post-transfusion hepatitis, and several other designations which weren’t very useful.
Shown here is a timeline of post-transfusion hepatitis, a major clinical problem in the post war era as blood transfusions was widely accepted and became well-organized. The first big improvement in the rate of post-transfusion hepatitis was the discovery of the Australian antigen by Baruch Blumberg about 1970, a discovery which allowed screening of donor blood. The rate of post-transfusion hepatitis in the United States in 1965 was about 22%. So the blood supply was not very clean. A big issue then was heavy reliance on professional blood donors, about 40 % of whom were infected with a hepatitis B or C. .
Screening of donated blood for virus infections picked up with anti-HIV testing because some of those donors were affected by hepatitis viruses as well. the next step in screening ALT and AST to screen donated blood. The final step in making the blood supply safe was the introduction of screening for HCV in the 1990s.
The HCV story started with the discovery at the NIH of the so-called non-A, non-B hepatitis which subsequently was re-named hepatitis C. The virus was identified in 1989, and this led to the development of a screening test for test blood donors. Interferon therapy started in the early ’90s and then the big revolution in the last 20 years occurred around 2014 with approval of direct acting anti-viral drugs. It is predicted that HCV will eventually disappear about 2030.
These four researchers found a single clone of DNA in a sample of blood from a patient with nonA nonB post-transfusion hepatitis. This seminal discovery eventually led to isolation of the HCV, followed by complete genetic sequencing.
The global burden of HCV is huge disease, with about 2% of the world’s population being infected. This map shows the geographic distribution:: the redder the color the more prevalent the infection.
Initial infection with HCV can produce a number of different outcomes. The unusual thing about hepatitis C is the very high rate of chronic hepatitis. We learned that about 20% of acutely infected patients recovered but about 80% developed chronic infection with serious complications. including cirrhosis and hepatocellular carcinoma developing decades after infection, usually in individuals who were asymptomatic.
This slide shows a timeline of the treatment starting on the left in the early 90s with interferon, first for six months, then for 12 months. And then the addition of ribavirin which increased clearance from the blood of HCV. And eventually introduction of pegylated interferon, and finally the current agents of choice, the direct acting anti-viral drugs. Currently about 100% of people with infection can be cured by these powerful medications.
A lot of the clinical research on HCV eradication has taken place here at BIDMC, much of it under the leadership of Nid Afdhal and his colleagues who published this paper in the New England Journal in 2014. This landmark study was the first randomized trial demonstrating cure of HCV infection with all oral direct acting antiviral therapy with these two DAAs, together known as Harvoni. Currently, we’re at the point where this condition can be cured. These new drugs have revolutionized our approach to this silent killer.
Howard Gruber was a psychologist who studied the processes and backgrounds of discovery and invention. He wrote: “The power of the beauty of science,” I think you can substitute “medicine” there, “do not rest upon infallibility, which it has not, but on corrigibility, without which it is nothing.” Corrigibility, or correctability derived from the Latin word corrigere, “to correct.” I have shown examples of how previous medical paradigms have been corrected and replaced. As I mentioned at the beginning of my lecture most of what I learned about Gastroenterology in my early training at UCLA has been corrected. And the same will happen to you. So what you’re learning now is as correct as we can make it, but eventually it will be replaced. So stay tuned.
For more information, see the video of the slides (includes audio). J. Thomas Lamont MD’s bio.